Gastroschisis: Baby Care & Recovery Guide 2026
Finding out that your unborn baby has gastroschisis can be emotionally difficult. Many parents immediately search for what gastroschisis is and whether their baby will survive. Gastroschisis is a birth defect during pregnancy where a baby is born with an abdominal wall defect, causing organs outside the body, usually the intestines, to be outside the abdomen, through a hole beside the belly button. This condition develops due to a fetal development abnormality in early fetal development.
The good news is that modern gastroschisis treatment and neonatal surgery have greatly improved gastroschisis survival and gastroschisis prognosis. With early prenatal detection, expert hospital specialists, and dedicated neonatal intensive care unit (NICU) support, most babies recover and grow normally.
What Is Gastroschisis? A Simple Explanation for Parents
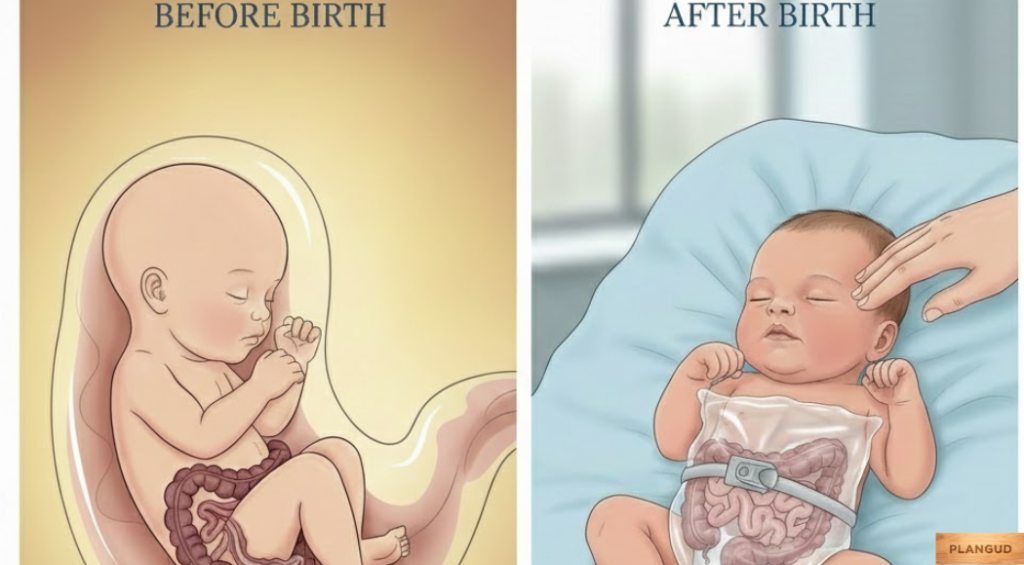
Gastroschisis in babies means a newborn is born with their intestines protruding outside the body through an opening in the abdominal wall. Unlike an omphalocele, there is no membrane covering the exposed organs. Because of amniotic fluid exposure, the intestines may become swollen or even twisted before birth. Immediately after delivery, doctors protect the organs and prepare the baby for gastroschisis surgery to place them back inside the body.
Why Gastroschisis Happens: Causes and Risk Factors
Many parents ask about the causes. The direct cause of birth defect, but research from organizations like the Centers for Disease Control and Prevention (CDC) shows certain maternal risk factors. These include young maternal age risk, tobacco and alcohol risk, and some environmental exposures. However, gastroschisis can occur in any pregnancy, even with good pregnancy care, so parents should never blame themselves.
Symptoms and Early Detection During Pregnancy
There are usually no physical gastroschisis symptoms felt by the mother. Instead, doctors identify the condition through ultrasound detection during routine prenatal tests. A fetal ultrasound shows the intestines outside the abdomen. Sometimes a blood screening test, especially an alpha-fetoprotein test, suggests a possible gastroschisis diagnosis. In selected cases, MRI pregnancy imaging using magnetic resonance imaging (MRI) provides more detail for delivery planning.
Types of Gastroschisis and How They Differ
Most babies have simple gastroschisis, where only the intestines are outside the body. Complex gastroschisis involves intestinal blockage, bowel damage, or missing segments that may later require a bowel resection procedure, ileostomy, or colostomy surgery. Complex cases need longer NICU hospital stays, but specialized care still leads to positive outcomes.
Diagnosis of Gastroschisis Before and After Birth
A gastroschisis diagnosis is usually confirmed before birth through ultrasound imaging and prenatal monitoring. After delivery — whether by vaginal delivery or cesarean delivery — doctors immediately protect the organs, prevent hypothermia, and prepare for surgery. Babies are placed in a neonatal intensive care unit (NICU) with IV nutrition and careful monitoring.
Treatment Options for Babies Born With Gastroschisis
Gastroschisis treatment always involves surgery. If the baby’s abdomen can hold the organs, doctors perform a primary repair procedure, returning the intestines inside and closing the abdominal opening.
If the intestines are too swollen, a staged repair procedure is done. A silo bag medical device (also called silo pouch treatment) is placed over the exposed organs and gradually moves them into the abdomen over several days.
After intestinal surgery, babies receive intravenous (IV) line nutrition and sometimes nasogastric tube feeding until normal feeding after surgery begins.
Risks and Complications Associated With Gastroschisis
Possible digestive system complications include surgical site infection, intestinal blockage, or slow bowel function. Rarely, children develop short bowel syndrome if parts of the intestine are missing or damaged. Close post-surgery recovery care in the NICU helps doctors detect and treat complications early.
Prognosis and Survival Rates for Newborns
Today, gastroschisis survival rates are high in hospitals with pediatric surgical teams. If gastroschisis is the only health condition, the gastroschisis prognosis is excellent. Early prenatal detection, experienced surgeons, and modern NICU care have transformed outcomes over the last decade.
Long-Term Outlook and Digestive Health Development

Most children achieve normal digestive health development and a positive long-term digestive outlook. Some may experience mild digestion sensitivity, but regular follow-ups with a pediatric healthcare provider ensure healthy growth.
Living With Gastroschisis: Daily Care and Feeding Support
After discharge, parents receive guidance on wound care, breastmilk feeding after surgery, and recognizing warning signs. Over time, babies transition to normal feeding, and families return to everyday life with confidence and routine.
Lifestyle and Dietary Adjustments After Surgery
Most children eat a normal diet. In rare cases of bowel shortening, doctors advise special nutrition plans. A balanced diet, pregnancy, and healthy infant nutrition support long-term recovery.
You may also like: plangud
Preventive Measures and Maternal Care During Pregnancy
While not all cases are preventable, good maternal prevention steps reduce overall birth defect risks. Mothers are advised to avoid smoking during pregnancy, avoid alcohol during pregnancy, attend regular prenatal tests, and maintain healthy pregnancy care.
Coping Strategies for Parents and Families

Emotional stress is normal. Support groups, medical teams, and parent coping strategies help families manage anxiety. Trusting your doctors and staying informed builds strength during your baby’s recovery journey.
Conclusion
A newborn diagnosis can feel frightening, but modern gastroschisis surgery, expert NICU care, and ongoing medical support provide real hope. With early gastroschisis diagnosis, proper gastroschisis treatment, and committed hospital specialists, most babies grow up healthy. Understanding the condition transforms fear into confidence and reassures parents that recovery is not only possible but highly expected.
FAQs
1. Is gastroschisis a high-risk pregnancy?
Yes — a pregnancy complicated by gastroschisis is considered high risk because the baby has an abdominal wall defect that requires expert prenatal monitoring and delivery planning. Specialists in maternal-fetal medicine often manage care to optimize outcomes for both mother and baby.
2. How long does it take to recover from gastroschisis?
Recovery time varies, but many babies stay in the neonatal intensive care unit (NICU) for 2–8 weeks after birth and surgery. Full recovery depends on how quickly the intestines start working and the absence of complications.
3. What happens if a woman gives birth to a baby with gastroschisis?
After delivery, the baby’s exposed organs are protected and evaluated, then a surgical repair (primary or staged) is performed to place the organs inside the abdomen. Specialized care in the NICU follows, with support for feeding and healing.
4. Can gastroschisis cause problems later in life?
Most children with gastroschisis grow up healthy, but a small number may have long-term digestive issues like intestinal blockage or slow digestion. Regular follow-up with a pediatric healthcare provider helps manage any ongoing concerns.
5. Can stress cause gastroschisis?
There is no scientific evidence that emotional stress directly causes gastroschisis. The condition is linked to early fetal development abnormalities, and known risk factors include young maternal age and certain lifestyle exposures, not stress.
6. What country has the highest rate of birth defects?
Birth defect rates vary worldwide due to differences in reporting and prenatal care, but low- and middle-income countries often report higher overall rates due to limited access to prenatal screening and nutrition support. Specific comparisons can change yearly and depend on national health data standards.

